👉 Register for Free. Snoring, Heart Risks & Relationships: The Valentine’s Day Sleep Talk
– Upcoming Webinar on Feb 13th with Dr. Wells.

Home Sleep Apnea Testing: A Convenient Alternative to Lab Testing
What is Home Sleep Apnea Testing?
For many individuals, the notion of participating in a sleep study within a clinical laboratory may conjure images of tangled wires and sleepless nights in an unfamiliar setting. Sleep apnea, a prevalent disorder with potentially severe implications if left untreated, has traditionally necessitated such overnight laboratory-based assessments for diagnosis. However, technological advancements now present a more convenient alternative: home sleep apnea testing (HSAT).
Sleep apnea—characterized by recurrent pauses in breathing during sleep—affects millions globally and manifests in various forms, including obstructive sleep apnea, central sleep apnea, and complex sleep apnea. Understanding these distinctions is essential for determining appropriate diagnostic and treatment strategies. As awareness of this disorder increases, so does the demand for accessible testing methods that integrate seamlessly into our increasingly busy lives.
This article will examine the emerging trend of home sleep apnea testing as a practical and comfortable alternative to conventional lab-based sleep studies. We will explore the mechanics of HSAT, its benefits, and its limitations, and compare its effectiveness with traditional methods. Our aim is to assist you in making an informed decision regarding whether this at-home approach is the most suitable choice for you.
Understanding Sleep Apnea
Sleep apnea is a prevalent sleep disorder characterized by repetitive episodes of apnea, or pauses in breathing, and reduced airflow during sleep due to upper airway obstruction. This condition can significantly disrupt sleep patterns, affecting overall sleep health and leading to excessive daytime sleepiness, impaired cognitive function, and an increased risk of accidents. Traditionally, diagnosing sleep apnea involved an overnight, attended sleep study known as polysomnography, conducted in a clinical setting such as a sleep lab or center. However, the advent of home sleep apnea testing offers a more convenient, cost-effective alternative for diagnosing obstructive sleep apnea in select patients. The results from these studies are crucial in understanding the presence and severity of the disorder, which in turn guides the appropriate treatment decisions to improve sleep medicine outcomes..
Types of Sleep Apnea
Sleep apnea is generally classified into two main types: obstructive and central. Each type has distinct characteristics and requires specific approaches for diagnosis and management.
- Obstructive Sleep Apnea (OSA):
- Description: OSA is characterized by the collapse or blockage of the airways during sleep, leading to breathing interruptions.
- Diagnosis: It is commonly diagnosed using home sleep apnea tests, which monitor sleep patterns, blood oxygen levels, and breathing irregularities.
- Central Sleep Apnea (CSA):
- Description: CSA occurs when the brain fails to send proper signals to the muscles that control breathing. This type of sleep apnea is less prevalent.
- Diagnosis: Due to its complexity, CSA is not typically diagnosed with at-home tests but requires a sleep study in a lab or sleep center.
Individuals with symptoms or a history of related diseases should consult a sleep specialist. Devices like the WatchPAT can detect both types but are mostly used for OSA analysis. For comprehensive assessment, especially in the presence of heart or pulmonary diseases, lab-based polysomnography is recommended.
| Type of Sleep Apnea | Description | Common Diagnosis Method |
| Obstructive Sleep Apnea (OSA) | Airway blockage during sleep | Home Sleep Apnea Test |
| Central Sleep Apnea (CSA) | Brain’s failure to signal breathing | Lab-based Sleep Testing |
What is Home Sleep Apnea Testing (HSAT)?
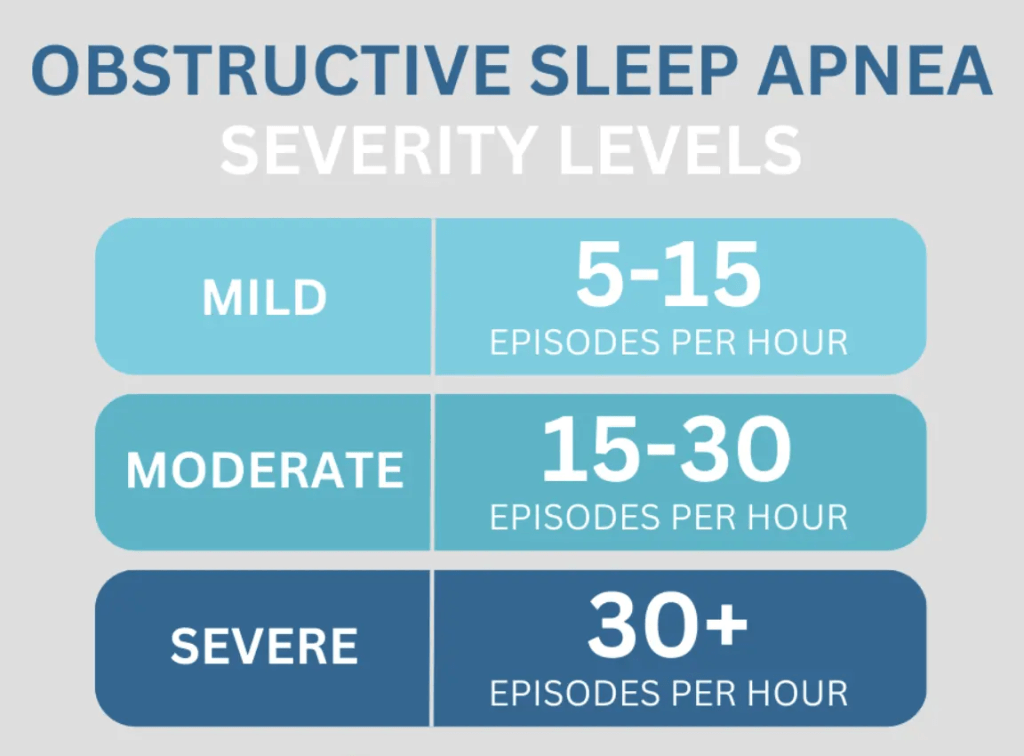
Home Sleep Apnea Testing (HSAT) is an innovative method designed to diagnose obstructive sleep apnea (OSA) from the comfort of a patient’s home. This approach utilizes a portable breathing monitor worn overnight to assess and record the individual’s breathing patterns, detect pauses or apneas during sleep, and measure blood oxygen levels. These insights are crucial in understanding the frequency and severity of respiratory disruptions, as the test calculates the average number of respiratory lapses per hour.
This method is increasingly favored due to its convenience and cost-effectiveness, particularly for those suspected of having mild to moderate sleep apnea. Once the data is collected, it’s uploaded to a secure server, allowing a sleep medicine specialist to interpret the results and provide an accurate diagnosis. HSAT stands as a practical solution for those hesitant or unable to participate in lab-based studies, bringing essential diagnostic tools into the comfort of one’s home.
Key Features of HSAT
HSATs are streamlined devices that serve as efficient tools for individuals needing evaluation for obstructive sleep apnea. These monitors primarily focus on tracking breathing patterns, oxygen levels, and the effort required to breathe, though they do not provide a complete picture of overall sleep quality or reveal detailed sleep patterns. The procedure begins with a consultation from a healthcare provider, followed by obtaining the testing equipment.
Patients wear the devices overnight before returning them for review. The results are then analyzed with a healthcare professional. Particularly suitable for those likely to have moderate to severe OSA without additional complications, these tests integrate modern technology, such as Bluetooth and mobile apps, to ensure data is seamlessly transmitted for specialist assessment.
At SLIIIP we offer different home sleep tests depending on the type of insurance the patients has. We verify benefits before we start the sleep treatment process so the patient is aware of the costs and what insurance will cover. Dr. Avinesh Bhar
Differences from Lab-Based Sleep Studies
Home sleep apnea tests and lab-based sleep studies differ significantly in scope and application. Primarily, HSATs focus on nighttime breathing and involve fewer sensors, meaning they measure fewer physiological parameters compared to comprehensive lab studies.
While home testing allows individuals to sleep in their familiar environment, offering a level of comfort not present in lab settings, it can also lead to limitations. HSATs are typically suggested for individuals with a strong likelihood of having mild to moderate OSA, whereas lab-based tests cater to a broader array of sleep disorders.
Moreover, lab studies offer more extensive data collection through a wider assortment of sensors that can capture sleep staging and other complex sleep variables. However, lab tests can sometimes present logistical challenges and involve higher costs. Conversely, one drawback of HSAT is its potential to underestimate the severity of sleep apnea. Therefore, while convenient, HSATs may not always provide as complete a diagnosis as an in-lab polysomnography would.
Benefits of Home Sleep Apnea Testing
The advent of home sleep apnea testing has significantly transformed the landscape of diagnosing sleep-disordered breathing, particularly conditions like Obstructive Sleep Apnea (OSA).
This approach offers numerous benefits, making it an increasingly popular choice for both patients and healthcare providers. By allowing individuals to conduct the test in their own home, patients can maintain their usual sleep patterns, free from the constraints of a clinical environment. This not only enhances the accuracy of data collected, such as breathing efforts and oxygen levels, but also improves the patient experience.
Additionally, home sleep studies can be carried out over multiple nights, providing a more comprehensive picture of sleep health. With many health insurance plans, including Medicare Part B, offering coverage for these tests, home sleep studies are an attractive, cost-effective alternative to traditional methods. Let’s explore these benefits further under the sections of convenience and comfort, cost-effectiveness, and faster diagnosis process.
Convenience and Comfort
Home sleep apnea testing stands out for its convenience and comfort, offering a hassle-free alternative to traditional sleep lab experiences. Instead of spending the night in an unfamiliar clinic, patients can complete the test from the comfort of their own bed, which naturally aligns with their sleep patterns.
This method not only enhances the patient’s comfort but also improves the authenticity of the results, as individuals can maintain their typical nighttime routines.
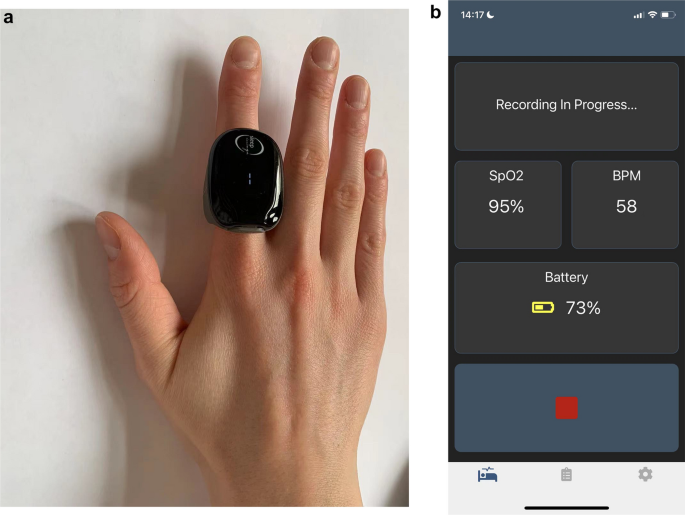
Modern technology, such as the WatchPAT device, simplifies the testing process, allowing patients to easily monitor their breathing and oxygen levels from home. Typically, a quick in-office appointment is arranged to educate patients on using the device, after which they are free to conduct the test overnight at their convenience. This approach eliminates the need for potentially stressful overnight clinic stays, making the entire diagnostic process more pleasant and patient-friendly.

Cost-Effectiveness
One of the most compelling aspects of home sleep apnea testing is its cost-effectiveness. Compared to traditional lab-based sleep studies, which can range from $1,000 to $7,000, home sleep tests are significantly more affordable, typically costing between $150 to $500 in the U.S. This price difference makes home testing an attractive first-line diagnostic tool for sleep-disordered breathing. Health insurance providers often favor home sleep tests, as many of them cover a portion—or even the entirety—of the costs, though patients may still need to meet any outstanding deductibles.
Faster Diagnosis Process
The expedited nature of home sleep apnea tests is another significant benefit, providing patients with quicker access to vital diagnostic information. Traditional sleep labs often involve longer wait times, from booking the appointment to receiving results, due to the need for in-clinic overnight stays and more complex logistical arrangements.
In contrast, home testing can be administered swiftly, allowing patients to bypass extended wait times for a more rapid diagnosis. At SLIIIP patients can often get appointments booked in 7 days and start their home sleep test in less than 10 days.
This quicker turnaround is crucial for those suffering from Obstructive Sleep Apnea, as it enables a faster start to necessary treatment interventions. Insurance often covers at-home testing, facilitating a seamless and faster diagnostic process that alleviates the delay commonly associated with sleep center appointments. By reducing wait times and expediting diagnosis, home sleep studies empower patients to take control of their sleep health more promptly and effectively.
How HSAT Works
Home Sleep Apnea Testing (HSAT) provides a user-friendly and cost-effective approach to diagnosing obstructive sleep apnea (OSA) at home. HSAT utilizes a portable breathing monitor that tracks essential health indicators overnight. This method is particularly beneficial for those who suspect they have moderate to severe OSA, as it circumvents the need for attending in-lab sleep studies. The HSAT device records the frequency of breathing lapses, known as apneas, to determine the severity of sleep apnea. After collecting data at home, the information is analyzed by healthcare providers to form an accurate diagnosis and informed treatment plan. This seamless integration of technology into home environments not only enhances convenience but also promotes more people seeking a diagnosis who might otherwise avoid testing due to logistical concerns.
Measuring Airflow
Measuring airflow is a critical element of Home Sleep Apnea Testing, where simplified devices assess breathing patterns during sleep. These tests typically utilize basic sensors to detect airflow, heart rate, and blood oxygen levels.
Although less comprehensive than overnight studies like nocturnal polysomnography conducted in sleep labs, home tests offer convenience and ease of use. The accuracy of these devices can vary, and they may employ nasal pressure transducers and oronasal thermal airflow sensors to detect apneas. While home tests may not provide as detailed information as professional sleep lab equipment, they are generally reliable for identifying significant sleep apnea. This makes them suitable for those with a moderate to high risk of OSA who seek a preliminary evaluation of their condition.
Monitoring Breathing Patterns
Monitoring breathing patterns is another essential function of HSAT devices. These simplified devices measure a variety of indicators, including heart rate, blood oxygen levels, and airflow to offer insights into breathing irregularities. Unlike in-lab studies, home tests usually do not monitor brainwaves, which can limit their ability to assess overall sleep quality. The process involves obtaining the home sleep apnea test equipment from a healthcare provider, conducting the test overnight at home, and returning the device for analysis. Some home devices might include advanced sensors for optional measurements, such as EEG or ECGs, depending on individual clinical recommendations. Advanced portable devices like the WatchPAT gather comprehensive data by contacting multiple body points, thus enhancing the accuracy of breathing pattern assessments.
Tracking Oxygen Levels
Tracking blood oxygen levels is a crucial aspect of Home Sleep Apnea Testing, primarily classified as type 3 or type 4 tests. Type 3 tests specifically measure oxygen saturation using various sensors, offering a broader range of data collection compared to type 4 tests. The WatchPAT device exemplifies a sophisticated approach, recording not only oxygen saturation but also providing extensive diagnostic capabilities. Accurate oximetry or assessment of blood oxygen levels plays an essential role in recognizing sleep apnea, with devices incorporating pulse oximeters for precision. These tools are part of the standard monitoring process in home sleep tests, ensuring that oxygen saturation levels are meticulously recorded to aid in diagnosis. This aspect of HSAT is vital in creating a full spectrum analysis of sleep-disordered breathing events.
Limitations and Considerations
Home sleep apnea tests (HSATs) provide a convenient and accessible option for diagnosing sleep apnea, especially for individuals already suspected of having moderate to severe Obstructive Sleep Apnea (OSA). However, while these tests offer the benefit of being administered in the comfort of one’s home, they have significant limitations. Unlike in-lab sleep studies that monitor brain waves, HSATs lack the capacity to measure the quality of sleep directly, which can affect the accuracy of diagnoses.
Additionally, HSATs do not involve a healthcare professional during the test, increasing the potential for errors or malfunctions. These limitations necessitate careful consideration and understanding of when HSATs might not be the best diagnostic tool, paving the way for cases where in-lab evaluations are more suitable.
Situations Where HSAT May Fall Short
There are instances where Home Sleep Apnea Testing may not provide a complete picture of a patient’s sleep health. One significant concern is the way these tests estimate the severity of sleep apnea. By calculating respiratory event frequency based on the total time a person spends in bed, rather than actual sleep time, HSATs can underestimate the apnea hypopnea index. This miscalculation may result in a less accurate classification of sleep apnea severity, potentially leading to inappropriate treatment recommendations.
Furthermore, depending on proper application and functionality, HSAT devices can yield inaccurate results when not handled correctly. Malfunctions or errors without healthcare professional oversight may compromise the reliability of the data. Patients with complex conditions like lung disease or heart failure are generally unsuitable candidates for HSAT, which might lead to a misdiagnosis or under-diagnosis of sleep disorders. Without brain wave monitoring, HSATs may also misdiagnose sleep apnea severity or confuse it with simple snoring.
When Further Evaluation is Necessary
Despite the convenience and accessibility of HSATs, there are scenarios where more thorough investigation is crucial. For patients with complex neurological or cardiopulmonary conditions, an in-center, overnight sleep study may be more appropriate. HSATs can sometimes miss milder forms or variations of sleep apnea, as they rely on indirect measurements that might not fully capture the patient’s sleep patterns. In such cases, patients might exhibit symptoms like excessive daytime sleepiness that are not thoroughly explained by HSAT results.
When symptoms persist despite HSAT findings, consulting a sleep medicine specialist is advisable. These professionals can determine whether further evaluation is warranted, possibly recommending an in-lab sleep study at a sleep lab. This more comprehensive evaluation can provide a clearer understanding of sleep-disordered breathing events, offering a more tailored approach to treatment. Ultimately, the decision to conduct further studies should focus on providing the most accurate diagnosis and effective treatment plan for each individual.
Comparing HSAT and Lab-Based Testing
With an increasing focus on accessibility and affordability in healthcare, home sleep apnea tests (HSAT) offer a convenient alternative to traditional in-laboratory sleep studies for diagnosing obstructive sleep apnea (OSA). HSAT is particularly suitable for individuals presenting clear symptoms of sleep disorder, such as partner-reported snoring and excessive daytime sleepiness, but without complex medical conditions. Moreover, HSAT can capture up to 98% of sleep apnea cases, costing significantly less and being eligible for Health Savings Account (HSA) or Flexible Spending Account (FSA) reimbursement. However, the tests may underestimate the severity of the condition. In contrast, in-laboratory polysomnography (PSG) remains the gold standard for situations where HSAT results are negative despite a strong suspicion of sleep apnea. It provides a comprehensive analysis of sleep patterns, including measurements that HSAT might miss, such as periodic limb movements
Accuracy and Reliability
The accuracy of HSAT varies between 68% and 91%, hinging on the type of monitoring device and the individual’s risk level for OSA. These tests are generally more reliable for individuals at higher risk, such as those with pronounced symptoms or obesity. However, HSATs have limitations in scope, mainly due to their reliance on estimated sleep time rather than continuous observation. This can sometimes lead to misdiagnosis or underestimation of the apnea’s severity, especially in cases of mild sleep apnea or other disorders like narcolepsy or periodic limb movement disorder. Nonetheless, when conducted properly, HSAT serves as a dependable diagnostic tool for moderate to severe OSA in uncomplicated adult patients.
Situational Suitability
HSAT is particularly suited for individuals who have a high risk of moderate to severe obstructive sleep apnea. It’s an appropriate choice for patients who do not have underlying health conditions such as lung disease, heart failure, or complex sleep disorders that might complicate the test’s results. The primary use of HSAT is to detect sleep-disordered breathing issues rather than other sleep disorders requiring comprehensive brain wave measurements. Health professionals often use criteria like the STOP-BANG checklist—a quick assessment tool considering factors such as snoring, observed apneas, daytime fatigue, and high blood pressure—to determine if an HSAT is suitable for a patient. Conversely, these tests are not generally recommended for children due to limitations in capturing the nuanced sleep disorders that can occur in younger patients, a stance supported by guidelines in the Journal of Clinical Sleep Medicine.
Steps to Take After HSAT
Completing a home sleep apnea test (HSAT) is an important step in diagnosing obstructive sleep apnea (OSA) and understanding your sleep health. If your test results are inconclusive or negative, it is crucial to consult with a healthcare provider to determine the appropriate next steps. Often, healthcare professionals may recommend undergoing a more comprehensive sleep study, such as polysomnography, at a sleep lab to gather more granular data. This in-lab testing can provide a clearer picture by tracking brain waves and actual sleep time, which are not monitored by home tests. It is not uncommon for symptoms and test results to advocate additional clinical evaluations, especially if there is suspicion of other health conditions like central sleep apnea. Before proceeding, it is advisable to check with your insurance provider, as coverage for these follow-up actions can vary. A collaborative discussion with your doctor will guide you in making informed decisions, potentially incorporating lifestyle changes or medical interventions if required.
Interpreting Results
After completing a home sleep apnea test, interpreting the results is a critical step in managing your sleep health. This type of test primarily monitors your breathing patterns, blood oxygen levels, heart rate, and air movement. It does not, however, measure brain waves or actual sleep time. The accuracy of home sleep apnea tests can vary substantially, largely depending on the device used and the individual’s assessed risk level for sleep apnea. When discussing the results, you’ll typically receive an OSA severity score, indicating the average number of breathing lapses per hour in bed. It is essential to ensure the correct usage of sensors placed on the finger, wrist, and chest to achieve accurate results. While these tests are effective at identifying obstructive sleep apnea, they do have limitations in detecting other complex sleep disorders. Therefore, understanding what your specific results say about your health is crucial in formulating a possible treatment plan.

Discussing Outcomes with Healthcare Providers
Understanding and following up on home sleep apnea test outcomes with healthcare providers is a pivotal step in effectively managing sleep disorders. Healthcare providers, including pulmonologists and sleep medicine specialists, play a key role in reviewing HSAT records to identify any significant abnormalities. This collaboration often extends to involve a team of specialists, including neurologists and primary care professionals, to gather a complete medical history relevant to sleep apnea outcomes. Such teamwork ensures seamless and integrated care when discussing test results.
Healthcare providers strive to interpret data from home sleep apnea tests accurately to determine the appropriate treatment plans for managing various conditions. This process often involves cross-discussion among healthcare providers, making sure that all aspects of a patient’s health are considered. The follow-up appointments might involve discussing the findings of the home sleep apnea test in detail with multiple providers to offer a comprehensive approach to health management.
Through these discussions, healthcare providers help patients understand their condition better and explore treatment options such as positive airway pressure therapy, lifestyle changes, or further diagnostic evaluations in sleep centers. Patients should ensure they engage actively in these discussions to make informed decisions about their health and sleep patterns, ultimately improving their quality of life.
Who Should Consider HSAT?
Home sleep apnea testing (HSAT) provides an efficient and accessible way to diagnose sleep apnea in adults aged 18 or older. It is primarily recommended for patients who likely have moderate to severe obstructive sleep apnea (OSA) and require insurance approval to proceed with testing. An ideal candidate for HSAT has a high pretest probability of OSA, often evident through symptom assessments like the STOP BANG questionnaire. However, HSAT is not without its criteria; patients must have no significant co-morbid conditions such as advanced pulmonary or significant cardiac diseases, which could complicate the use of home-based testing. Moreover, HSAT is unsuitable for individuals with conditions like central sleep apnea or significant heart failure, as these require more comprehensive diagnostic measures. Understanding who benefits from HSAT and ensuring the appropriateness of this test can lead to better management of sleep disorders.
Patient Profiles Benefiting from HSAT
Certain patient profiles lend themselves well to home sleep apnea testing. Those with a history of partner-reported snoring, excessive tiredness during the day, and restlessness while sleeping are excellent HSAT candidates. These symptoms often indicate a higher risk of OSA, which HSAT effectively detects. Furthermore, individuals with conditions increasing cardiovascular risk, such as atrial fibrillation or nocturnal angina, may find HSAT beneficial due to its ability to identify sleep apnea’s impact on heart health. The convenience and accessibility of HSAT, where patients can receive the testing device with ease and perform it in their own homes, enhance the patient experience. At institutions like the Mayo Clinic Center for Sleep Medicine, HSAT has proven effective, diagnosing over 40% of patients with OSA due to its streamlined process. It’s crucial, however, that patients are capable of using the device unaided to ensure accurate results.
Conclusion
Home sleep apnea testing (HSAT) is a valuable tool for identifying moderate to severe obstructive sleep apnea (OSA) in patients without complicating disorders. By monitoring key indicators such as respiratory patterns, oxygen levels, heart rate, and airflow, HSAT plays an important role in diagnosing OSA, a condition marked by interrupted breathing during sleep. However, because HSAT focuses solely on breathing-related issues and does not capture brain wave activity, it cannot detect non-breathing-related sleep disorders like insomnia. Additionally, HSAT may underestimate apnea severity by misclassifying severe cases as mild due to incomplete data on actual sleep time. For this reason, clinical follow-up is essential to confirm findings, avoid underdiagnosis, and provide comprehensive care tailored to each patient’s needs.
Latest posts
-
Sleep Apnea Symptoms: Complete Guide to Warning Signs in Men, Women, and Children
Medically reviewed by SLIIIP Board-Certified Sleep Medicine Specialists | Last Updated: January 2026 Sleep apnea is a serious sleep disorder that causes your breathing to repeatedly stop and start during…
-
Do I Have Sleep Apnea?
Take This Clinically-Based Sleep Apnea Risk Assessment Based on the STOP-BANG Questionnaire and Epworth Sleepiness Scale | Last Updated: January 2026 IMPORTANT: The quiz “Do I Have Sleep Apnea” is…
-
CPAP Machine Costs Explained: A Complete Buyer’s Guide for 2026
If you have been diagnosed with sleep apnea and prescribed CPAP therapy, understanding the costs involved is an important part of planning your journey toward better rest. CPAP machines represent…
·
Get updates
Spam-free subscription, we guarantee. This is just a friendly ping when new content is out.


One response to “Home Sleep Apnea Testing: A Convenient Alternative to Lab Testing”
[…] health are closely linked. Inadequate sleep can increase anxiety, depression, and irritability.By improving sleep apnea symptoms and supporting healthy weight, GLP-1s can indirectly enhance mood, focus, and confidence. Patients […]