👉 Register for Free. Snoring, Heart Risks & Relationships: The Valentine’s Day Sleep Talk
– Upcoming Webinar on Feb 13th with Dr. Wells.

Sleep Apnea and Atrial Fibrillation: Role of the Cardiac Autonomic Nervous System
Sleep apnea and atrial fibrillation (AF) are two common health problems that are linked more closely than you might think. Often getting treatment from a sleep medicine clinic can improve central sleep apnea.
Prevalence of OSA and A.Fib
Approximately 6 million Americans have received a diagnosis of sleep apnea; however, the actual prevalence of this sleep disorder is believed to impact around 30 million individuals in the U.S. 56% of people aged 65 and above exhibit a high risk of developing obstructive sleep apnea. (1)
Atrial fibrillation (AFib) stands as the most frequently diagnosed arrhythmia in clinical settings. Estimates indicate that AFib affects between approximately 2.7 million to 6.1 million individuals in the United States, with projections suggesting this figure will increase to 12.1 million by 2030.
The Heart Rhythm Society says that patients with obstructive sleep apnea have increased risk to get afib. This includes irregular heartbeat, nocturnal arrhythmias and cardiovascular disease. Obstructive sleep apnea creates sleep disordered breathing events which causes high blood pressure and irregular heartbeat.

Understanding Sleep Apnea and afib
AFib disrupts the heart’s electrical signals, causing the upper chambers (atria) to quiver instead of contract properly. This irregularity can lead to increased risk to blood clotting, significantly increasing the risk of stroke. Common risk factors for sleep apnea and AFib include age, high blood pressure, diabetes, and existing heart disease.
On the other hand, sleep apnea, affecting millions globally, is marked by breathing interruptions during sleep. Often family history is a factor in OSA patients. Obstructive sleep apnea, the most common type, occurs due to blocked airways in the throat. Despite its prevalence, sleep apnea often goes undiagnosed, with symptoms like loud snoring, gasping for air, excessive daytime sleepiness, and fatigue.
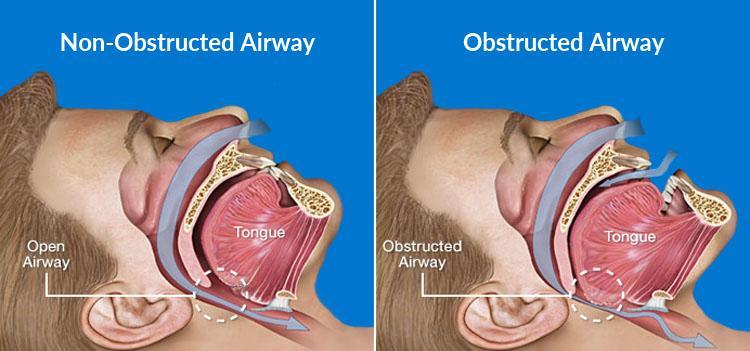
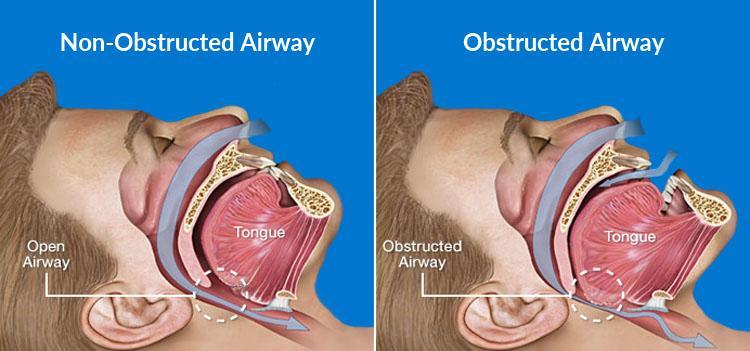
What is Obstructive Sleep Apnea?
Obstructive Sleep Apnea (OSA): is a sleep disorder characterized by episodes of upper airway obstruction during sleep, leading to pauses in breathing. These episodes can result in reduced oxygen levels in the blood and causes sleep disordered breathing. This can lead to cardiovascular disease and atrial fibrillation recurrence.
Obstructive sleep apnea reduces the amount of oxygen in the body. People with sleep apnea may snore, wake up unrefreshed from sleep or feel tired/fatigued during the day. They can also have respiratory disturbance and frequent awakening. Body mass index in patients with osa can be considered as other risk factors.
Prior diagnosis by a sleep doctor using sleep studies is a great way to get osa treatment. A sleep study can be done done at home using equipment that is sent from the sleep doctor. At Sliiip.com we have board-certified sleep doctors that can help you setup your first sleep study and is covered by major health insurances.
You can book your appointment with our clinical practice.
Diagnosing Sleep Apnea
Sleep apnea is often considered sleep disordered breathing and can cause heart rhythm issues. Untreated osa can lead to structural heart disease and pulmonary disease.
- Recognizing Symptoms: Be aware of common symptoms such as loud snoring, pauses in breathing during sleep, gasping or choking sensations, excessive daytime sleepiness, and morning headaches. If you or someone you know exhibits these signs, it’s important to consider the possibility of sleep apnea.
- Medical History Review: During an evaluation for sleep apnea, your healthcare provider will review your medical history, including any existing conditions, medications you’re taking, and lifestyle factors that may contribute to sleep disturbances.
- Sleep Study (Polysomnography): The gold standard for diagnosing sleep apnea is a sleep study, also known as polysomnography. This test is typically conducted in a sleep center or sometimes at home using portable monitoring devices. It measures various parameters during sleep, including breathing patterns, oxygen levels, heart rate, and brain activity.
- Home Sleep Apnea Testing: In some cases, if a patient is suspected of having uncomplicated obstructive sleep apnea, a healthcare provider may recommend a home sleep apnea test. This involves wearing a portable monitoring device at home to record breathing patterns, oxygen levels, and other relevant data during sleep. Sometimes an overnight sleep study is needed especially if there is sleep apnea severity.
- Clinical Evaluation: A healthcare provider, often a sleep medicine specialist or pulmonologist, will interpret the results of the sleep study or home sleep apnea test to make a diagnosis. They will also consider other factors such as physical examination findings and symptoms reported by the patient.
- Collaborative Treatment Planning: Once diagnosed with sleep apnea, collaborative treatment planning involves discussing treatment options with your healthcare provider. This may include lifestyle changes, such as weight loss or positional therapy, continuous positive airway pressure (CPAP) therapy, oral appliances, surgery, or other interventions tailored to individual needs.
What is Atrial Fibrillation (AF)?
Paroxysmal atrial fibrillation (AFib) describes a fast, irregular heartbeat that only lasts a few hours or days. Typically, it goes away on its own in under 24 hours, but it may last up to a week. Sometimes, people are unaware they have paroxysmal AFib
Atrial Fibrillation disrupts the heart’s electrical signals, causing the upper chambers (atria) to quiver and beat out of sync from the lower chambers (ventricles) of the heart. This causes the atria to not contract properly.
Symptoms of atrial fibrillation include palpitations (feeling the heart race), shortness of breath, tiredness, dizziness, and chest discomfort. AFib is dangerous and can lead to blood clotting, significantly increasing the risk of stroke.
In fact, A.Fib causes about 1 in 7 strokes and strokes associated with sleep apnea and AFib are found to be more severe. Common risk factors for AFib include age, high blood pressure, diabetes, and existing heart disease. According to the Stroke Association, atrial fibrillation recurrence can cause heart failure, increased blood pressure, acute hypercapnia and change your heart rhythm.

How They Are Connected
Research shows risk factors between sleep apnea, especially OSA, and atrial fibrillation. Here’s why:
- Nervous System Changes: Our nervous system is made up of two components, the autonomic AKA the “rest and digest” system and the sympathetic nervous system AKA the “fight or flight” response. Sleep apnea disrupts the autonomic nervous system, causing more ‘fight or flight’ responses during breathing pauses. This can trigger irregular heartbeats like AFib.
- Low Oxygen Levels: During sleep apnea episodes, oxygen levels drop in the blood, then go back up suddenly. This cycle stresses the heart and can lead to atrial fibrillation over time.
- Heart Strain: The ups and downs in oxygen levels and blood pressure during sleep apnea episodes strain the heart, making paroxysmal atrial fibrillation more severe.
What This Means for Treatment
Understanding the link between these conditions is key for effective treatment:
- Screening: People with AFib should be checked for sleep apnea, especially if they snore or feel very tired during the day.
- Treating Sleep Apnea: Using treatments like CPAP (a machine that helps keep airways open) can reduce how often AFib happens.
How does continuous positive airway pressure machine work?
- CPAP Machine: The core of the system is the CPAP machine, which generates a continuous stream of air at a prescribed pressure.
- Airflow Delivery: This pressurized air is delivered through a hose connected to a mask that covers the nose or both the nose and mouth.
- Keeping Airways Open: The steady flow of air from the CPAP machine prevents the airway from collapsing or becoming obstructed, ensuring that the user can breathe freely and continuously during sleep.
- Adjustable Pressure: The pressure setting on a CPAP machine is tailored to the individual’s needs, determined by a sleep study or consultation with a healthcare provider. Some CPAP machines automatically adjust the pressure throughout the night based on the user’s needs.
Does Sleep Apnea Treatment Improve AFib?
Yes, treating sleep apnea can significantly improve outcomes for patients with atrial fibrillation (AFib). Numerous studies have demonstrated the link between sleep apnea and AFib, and treating sleep apnea has been shown to reduce the recurrence of AFib, improve treatment efficacy, and enhance overall cardiovascular health. Here’s a detailed explanation of how sleep apnea treatment impacts AFib:
Mechanisms Linking Sleep Apnea and AFib:
- Intermittent Hypoxia: Sleep apnea causes repeated episodes of interrupted breathing, leading to intermittent hypoxia (low oxygen levels). This can induce oxidative stress and inflammation, which contribute to atrial remodeling and fibrosis, increasing the risk of atrial fibrillation.
- Sympathetic Activation: The frequent arousals from sleep and intermittent hypoxia lead to increased sympathetic nervous system activity, raising blood pressure and heart rate, which can trigger AFib.
- Intrathoracic Pressure Changes: The negative intrathoracic pressure during obstructive apneas can stretch the atrial walls, promoting atrial dilation and remodeling, further predisposing individuals to AFib.
- Increased Left Atrial Pressure: Sleep apnea can elevate left atrial pressure and volume, contributing to atrial enlargement and remodeling, which are key risk factors for AFib.

Impact of Sleep Apnea and afib Treatment:
- Reduction in AFib Recurrence:
- Continuous Positive Airway Pressure (CPAP) Therapy: CPAP is the most common and effective treatment for obstructive sleep apnea. Studies have shown that patients with AFib who adhere to CPAP therapy have significantly lower rates of atrial fibrillation recurrence compared to those who do not use CPAP. Obstructive sleep apnea can be fixed with cpap treatment.
- Ablation Outcomes: Patients undergoing catheter ablation for AFib who also treat their sleep apnea with CPAP have better procedural success rates and lower AFib recurrence rates.
- Improvement in Symptom Control:
- Treating sleep apnea can lead to better overall symptom control for patients with atrial fibrillation, including reductions in palpitations, fatigue, and exercise intolerance.
- Enhanced Cardiovascular Health:
- Treating sleep apnea can improve hypertension, reduce the risk of heart failure, and lower overall cardiovascular morbidity, which indirectly benefits AFib management.
- Reduction in Hospitalizations:
- Patients with both sleep apnea and atrial fibrillation who receive appropriate sleep apnea treatment tend to have fewer hospitalizations related to cardiovascular events.
Clinical Evidence:
- Study Findings:
- A study published in the Journal of the American College of Cardiology found that atrial fibrillation patients treated with CPAP had a 42% reduction in the recurrence of AFib compared to those who did not use CPAP.
- Another study in HeartRhythm journal showed that CPAP therapy (continuous positive airway pressure) was associated with improved outcomes after AFib catheter ablation, with a significant decrease in arrhythmia recurrence.
- Guidelines and Recommendations:
- Clinical guidelines from cardiology and sleep medicine societies recommend screening for sleep apnea in patients with atrial fibrillation and treating it as part of a comprehensive management plan for AFib.
Book a meeting for Treatment
At SLIIIP, we’re excited to provide sleep telemedicine services designed for your convenience and ease. Our sleep specialists offer online video consultations, utilize FDA-approved sleep tests, and conduct virtual therapy sessions to ensure you receive comprehensive and effective care.
I am Doctor Avinesh Bhar and me and my team of board-certified doctors are happy to help patients with OSA treatment.
Conclusion
By diagnosing and treating OSA in patients with atrial fibrillation we can help further reduce their risk of stroke and other complications. By treating sleep apnea, we can also improve how atrial fibrillation is managed. More research will help us understand this link even better and improve outcomes for people with both conditions.
Citations/Sources:
1. National Council on Aging (NCOA). (5/8/2024). Sleep apnea statistics. Retrieved from https://www.ncoa.org/adviser/sleep/sleep-apnea-statistics/#:~:text=Approximately%2039%20million%20U.S.%20adults,have%20mild%20to%20severe%20OSA
2. Centers for Disease Control and Prevention. (10/14/2022). Atrial Fibrillation (AFib) Fact Sheet. Retrieved from https://www.cdc.gov/heartdisease/atrial_fibrillation.htm3. Cantillon, D., & Amuthan, R. (2018, August). Atrial Fibrillation. Atrial fibrillation. https://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/atrial-fibrillation/
Sleep apnea and atrial fibrillation (AF) are two common health problems that are linked more closely than you might think. Often getting treatment from a sleep medicine clinic can improve central sleep apnea.
Prevalence of OSA and A.Fib
Approximately 6 million Americans have received a diagnosis of sleep apnea; however, the actual prevalence of this sleep disorder is believed to impact around 30 million individuals in the U.S. 56% of people aged 65 and above exhibit a high risk of developing obstructive sleep apnea. (1)
Atrial fibrillation (AFib) stands as the most frequently diagnosed arrhythmia in clinical settings. Estimates indicate that AFib affects between approximately 2.7 million to 6.1 million individuals in the United States, with projections suggesting this figure will increase to 12.1 million by 2030.
The Heart Rhythm Society says that patients with obstructive sleep apnea have increased risk to get afib. This includes irregular heartbeat, nocturnal arrhythmias and cardiovascular disease. Obstructive sleep apnea creates sleep disordered breathing events which causes high blood pressure and irregular heartbeat.

Understanding Sleep Apnea and afib
AFib disrupts the heart’s electrical signals, causing the upper chambers (atria) to quiver instead of contract properly. This irregularity can lead to increased risk to blood clotting, significantly increasing the risk of stroke. Common risk factors for sleep apnea and AFib include age, high blood pressure, diabetes, and existing heart disease.
On the other hand, sleep apnea, affecting millions globally, is marked by breathing interruptions during sleep. Often family history is a factor in OSA patients. Obstructive sleep apnea, the most common type, occurs due to blocked airways in the throat. Despite its prevalence, sleep apnea often goes undiagnosed, with symptoms like loud snoring, gasping for air, excessive daytime sleepiness, and fatigue.
What is Obstructive Sleep Apnea?
Obstructive Sleep Apnea (OSA): is a sleep disorder characterized by episodes of upper airway obstruction during sleep, leading to pauses in breathing. These episodes can result in reduced oxygen levels in the blood and causes sleep disordered breathing. This can lead to cardiovascular disease and atrial fibrillation recurrence.
Obstructive sleep apnea reduces the amount of oxygen in the body. People with sleep apnea may snore, wake up unrefreshed from sleep or feel tired/fatigued during the day. They can also have respiratory disturbance and frequent awakening. Body mass index in patients with osa can be considered as other risk factors.
Prior diagnosis by a sleep doctor using sleep studies is a great way to get osa treatment. A sleep study can be done done at home using equipment that is sent from the sleep doctor. At Sliiip.com we have board-certified sleep doctors that can help you setup your first sleep study and is covered by major health insurances.
You can book your appointment with our clinical practice.
Diagnosing Sleep Apnea
Sleep apnea is often considered sleep disordered breathing and can cause heart rhythm issues. Untreated osa can lead to structural heart disease and pulmonary disease.
- Recognizing Symptoms: Be aware of common symptoms such as loud snoring, pauses in breathing during sleep, gasping or choking sensations, excessive daytime sleepiness, and morning headaches. If you or someone you know exhibits these signs, it’s important to consider the possibility of sleep apnea.
- Medical History Review: During an evaluation for sleep apnea, your healthcare provider will review your medical history, including any existing conditions, medications you’re taking, and lifestyle factors that may contribute to sleep disturbances.
- Sleep Study (Polysomnography): The gold standard for diagnosing sleep apnea is a sleep study, also known as polysomnography. This test is typically conducted in a sleep center or sometimes at home using portable monitoring devices. It measures various parameters during sleep, including breathing patterns, oxygen levels, heart rate, and brain activity.
- Home Sleep Apnea Testing: In some cases, if a patient is suspected of having uncomplicated obstructive sleep apnea, a healthcare provider may recommend a home sleep apnea test. This involves wearing a portable monitoring device at home to record breathing patterns, oxygen levels, and other relevant data during sleep. Sometimes an overnight sleep study is needed especially if there is sleep apnea severity.
- Clinical Evaluation: A healthcare provider, often a sleep medicine specialist or pulmonologist, will interpret the results of the sleep study or home sleep apnea test to make a diagnosis. They will also consider other factors such as physical examination findings and symptoms reported by the patient.
- Collaborative Treatment Planning: Once diagnosed with sleep apnea, collaborative treatment planning involves discussing treatment options with your healthcare provider. This may include lifestyle changes, such as weight loss or positional therapy, continuous positive airway pressure (CPAP) therapy, oral appliances, surgery, or other interventions tailored to individual needs.
What is Atrial Fibrillation (AF)?
Paroxysmal atrial fibrillation (AFib) describes a fast, irregular heartbeat that only lasts a few hours or days. Typically, it goes away on its own in under 24 hours, but it may last up to a week. Sometimes, people are unaware they have paroxysmal AFib
Atrial Fibrillation disrupts the heart’s electrical signals, causing the upper chambers (atria) to quiver and beat out of sync from the lower chambers (ventricles) of the heart. This causes the atria to not contract properly.
Symptoms of atrial fibrillation include palpitations (feeling the heart race), shortness of breath, tiredness, dizziness, and chest discomfort. AFib is dangerous and can lead to blood clotting, significantly increasing the risk of stroke.
In fact, A.Fib causes about 1 in 7 strokes and strokes associated with sleep apnea and AFib are found to be more severe. Common risk factors for AFib include age, high blood pressure, diabetes, and existing heart disease. According to the Stroke Association, atrial fibrillation recurrence can cause heart failure, increased blood pressure, acute hypercapnia and change your heart rhythm.

How They Are Connected
Research shows risk factors between sleep apnea, especially OSA, and atrial fibrillation. Here’s why:
- Nervous System Changes: Our nervous system is made up of two components, the autonomic AKA the “rest and digest” system and the sympathetic nervous system AKA the “fight or flight” response. Sleep apnea disrupts the autonomic nervous system, causing more ‘fight or flight’ responses during breathing pauses. This can trigger irregular heartbeats like AFib.
- Low Oxygen Levels: During sleep apnea episodes, oxygen levels drop in the blood, then go back up suddenly. This cycle stresses the heart and can lead to atrial fibrillation over time.
- Heart Strain: The ups and downs in oxygen levels and blood pressure during sleep apnea episodes strain the heart, making paroxysmal atrial fibrillation more severe.
What This Means for Treatment
Understanding the link between these conditions is key for effective treatment:
- Screening: People with AFib should be checked for sleep apnea, especially if they snore or feel very tired during the day.
- Treating Sleep Apnea: Using treatments like CPAP (a machine that helps keep airways open) can reduce how often AFib happens.
How does continuous positive airway pressure machine work?
- CPAP Machine: The core of the system is the CPAP machine, which generates a continuous stream of air at a prescribed pressure.
- Airflow Delivery: This pressurized air is delivered through a hose connected to a mask that covers the nose or both the nose and mouth.
- Keeping Airways Open: The steady flow of air from the CPAP machine prevents the airway from collapsing or becoming obstructed, ensuring that the user can breathe freely and continuously during sleep.
- Adjustable Pressure: The pressure setting on a CPAP machine is tailored to the individual’s needs, determined by a sleep study or consultation with a healthcare provider. Some CPAP machines automatically adjust the pressure throughout the night based on the user’s needs.
Does Sleep Apnea Treatment Improve AFib?
Yes, treating sleep apnea can significantly improve outcomes for patients with atrial fibrillation (AFib). Numerous studies have demonstrated the link between sleep apnea and AFib, and treating sleep apnea has been shown to reduce the recurrence of AFib, improve treatment efficacy, and enhance overall cardiovascular health. Here’s a detailed explanation of how sleep apnea treatment impacts AFib:
Mechanisms Linking Sleep Apnea and AFib:
- Intermittent Hypoxia: Sleep apnea causes repeated episodes of interrupted breathing, leading to intermittent hypoxia (low oxygen levels). This can induce oxidative stress and inflammation, which contribute to atrial remodeling and fibrosis, increasing the risk of atrial fibrillation.
- Sympathetic Activation: The frequent arousals from sleep and intermittent hypoxia lead to increased sympathetic nervous system activity, raising blood pressure and heart rate, which can trigger AFib.
- Intrathoracic Pressure Changes: The negative intrathoracic pressure during obstructive apneas can stretch the atrial walls, promoting atrial dilation and remodeling, further predisposing individuals to AFib.
- Increased Left Atrial Pressure: Sleep apnea can elevate left atrial pressure and volume, contributing to atrial enlargement and remodeling, which are key risk factors for AFib.

Impact of Sleep Apnea and afib Treatment:
- Reduction in AFib Recurrence:
- Continuous Positive Airway Pressure (CPAP) Therapy: CPAP is the most common and effective treatment for obstructive sleep apnea. Studies have shown that patients with AFib who adhere to CPAP therapy have significantly lower rates of atrial fibrillation recurrence compared to those who do not use CPAP. Obstructive sleep apnea can be fixed with cpap treatment.
- Ablation Outcomes: Patients undergoing catheter ablation for AFib who also treat their sleep apnea with CPAP have better procedural success rates and lower AFib recurrence rates.
- Improvement in Symptom Control:
- Treating sleep apnea can lead to better overall symptom control for patients with atrial fibrillation, including reductions in palpitations, fatigue, and exercise intolerance.
- Enhanced Cardiovascular Health:
- Treating sleep apnea can improve hypertension, reduce the risk of heart failure, and lower overall cardiovascular morbidity, which indirectly benefits AFib management.
- Reduction in Hospitalizations:
- Patients with both sleep apnea and atrial fibrillation who receive appropriate sleep apnea treatment tend to have fewer hospitalizations related to cardiovascular events.
Clinical Evidence:
- Study Findings:
- A study published in the Journal of the American College of Cardiology found that atrial fibrillation patients treated with CPAP had a 42% reduction in the recurrence of AFib compared to those who did not use CPAP.
- Another study in HeartRhythm journal showed that CPAP therapy (continuous positive airway pressure) was associated with improved outcomes after AFib catheter ablation, with a significant decrease in arrhythmia recurrence.
- Guidelines and Recommendations:
- Clinical guidelines from cardiology and sleep medicine societies recommend screening for sleep apnea in patients with atrial fibrillation and treating it as part of a comprehensive management plan for AFib.
Book a meeting for Treatment
At SLIIIP, we’re excited to provide sleep telemedicine services designed for your convenience and ease. Our sleep specialists offer online video consultations, utilize FDA-approved sleep tests, and conduct virtual therapy sessions to ensure you receive comprehensive and effective care.
I am Doctor Avinesh Bhar and me and my team of board-certified doctors are happy to help patients with OSA treatment.
Conclusion
By diagnosing and treating OSA in patients with atrial fibrillation we can help further reduce their risk of stroke and other complications. By treating sleep apnea, we can also improve how atrial fibrillation is managed. More research will help us understand this link even better and improve outcomes for people with both conditions.
Citations/Sources:
1. National Council on Aging (NCOA). (5/8/2024). Sleep apnea statistics. Retrieved from https://www.ncoa.org/adviser/sleep/sleep-apnea-statistics/#:~:text=Approximately%2039%20million%20U.S.%20adults,have%20mild%20to%20severe%20OSA
2. Centers for Disease Control and Prevention. (10/14/2022). Atrial Fibrillation (AFib) Fact Sheet. Retrieved from https://www.cdc.gov/heartdisease/atrial_fibrillation.htm3. Cantillon, D., & Amuthan, R. (2018, August). Atrial Fibrillation. Atrial fibrillation. https://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/atrial-fibrillation/
Latest posts
-
Sleep Apnea Symptoms: Complete Guide to Warning Signs in Men, Women, and Children
Medically reviewed by SLIIIP Board-Certified Sleep Medicine Specialists | Last Updated: January 2026 Sleep apnea is a serious sleep disorder that causes your breathing to repeatedly stop and start during…
-
Do I Have Sleep Apnea?
Take This Clinically-Based Sleep Apnea Risk Assessment Based on the STOP-BANG Questionnaire and Epworth Sleepiness Scale | Last Updated: January 2026 IMPORTANT: The quiz “Do I Have Sleep Apnea” is…
-
CPAP Machine Costs Explained: A Complete Buyer’s Guide for 2026
If you have been diagnosed with sleep apnea and prescribed CPAP therapy, understanding the costs involved is an important part of planning your journey toward better rest. CPAP machines represent…
·
Get updates
Spam-free subscription, we guarantee. This is just a friendly ping when new content is out.


One response to “Sleep Apnea and Atrial Fibrillation: Role of the Cardiac Autonomic Nervous System”
The information you have provided here has helped me understand the correlation. Thank you doctor!